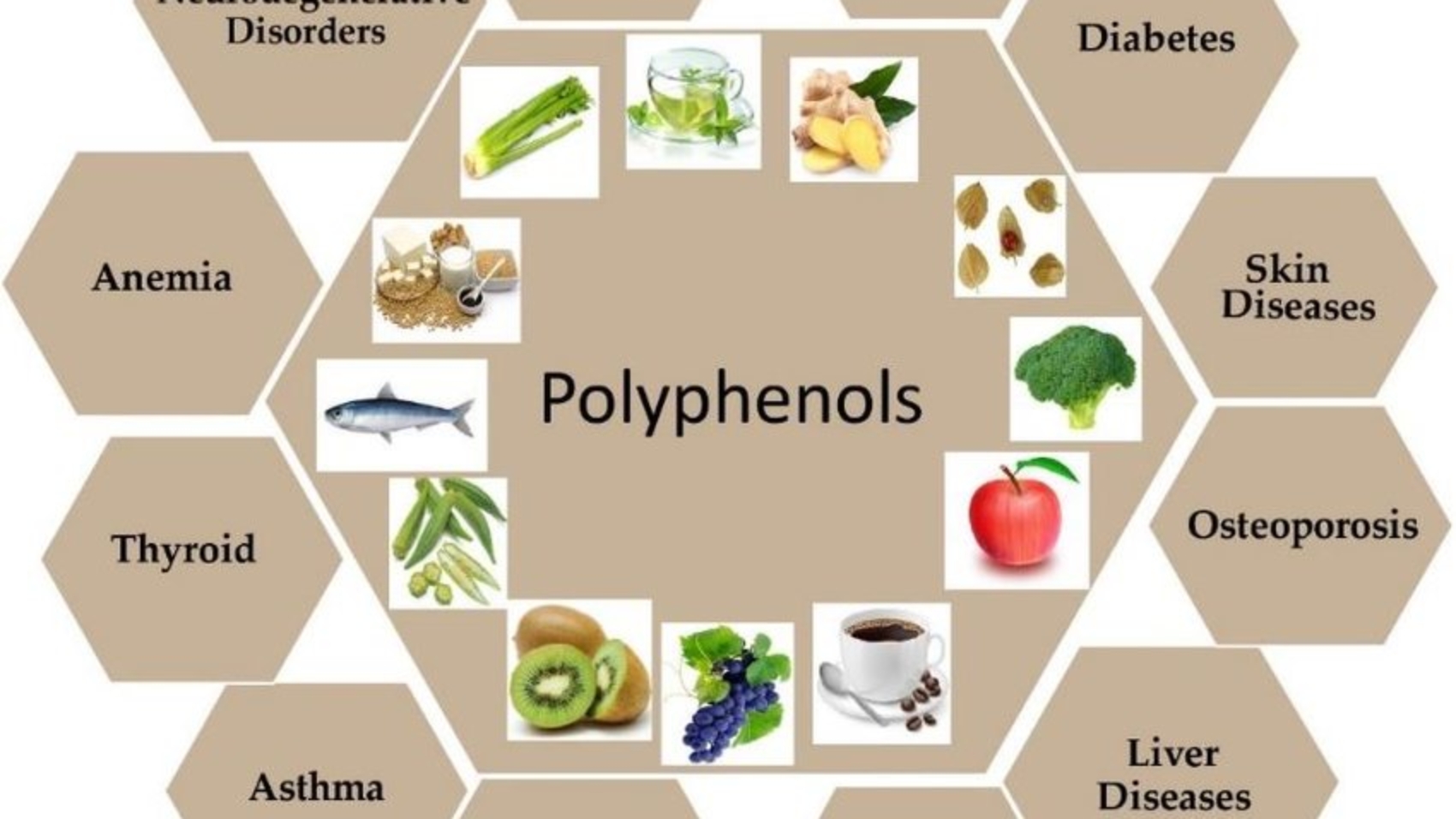
In the constantly evolving world of gut health, a fascinating topic gaining momentum is the role of polyphenols as emerging prebiotics. Polyphenols, the hidden treasures found in the vibrant hues of fruits, vegetables, tea, coffee, and even red wine, have recently taken center stage in the world of gut health. As we discover the secrets of these natural compounds, their emerging role as prebiotics adds a new dimension to the understanding of digestive well-being.
Polyphenols are a diverse group of antioxidants, including flavonoids, phenolic acids, and polyphenolic amides. These compounds serve as potent defenders of our health, combating oxidative stress and inflammation within the body. What sets polyphenols apart in the context of gut health is their newfound status as prebiotics, a designation that signifies their ability to fuel the growth of beneficial bacteria in the gut.
The term “prebiotics” refers to non-digestible fibers that act as a nourishing banquet for the microscopic residents of our digestive system. Unlike probiotics, which introduce live bacteria into the gut, prebiotics empower the existing beneficial bacteria, fostering a harmonious and thriving gut microbiome.
Polyphenols, in their role as emerging prebiotics, go beyond their antioxidant properties. They play a vital role in promoting the growth of beneficial bacteria while inhibiting the proliferation of harmful microbes. This dual action creates an environment conducive to a balanced and resilient gut microbiome.
The significance of polyphenols as prebiotics lies in their ability to modulate the composition of the gut microbiota. By influencing the balance between various bacterial species, polyphenols contribute to a healthy and diverse microbial community. This modulation, in turn, enhances the overall functionality of the digestive system. Dr. Rasha El Naggar at Etara Wellness emphasizes the importance of polyphenols in our diet, highlighting their role in promoting a healthy gut microbiome and overall well-being. As we delve into the intricacies of polyphenols as prebiotics, it becomes evident that their impact extends beyond the gut.
Understanding Polyphenols
Polyphenols are natural compounds found in plants, encompassing a diverse group of antioxidants. There are several types of polyphenols, including flavonoids, phenolic acids, and polyphenolic amides. Rich sources of these compounds are fruits, vegetables, tea, coffee, and red wine.
Types of Polyphenols
1. Flavonoids: Widely distributed in fruits, vegetables, and beverages such as tea and red wine, flavonoids constitute a major subclass of polyphenols. These compounds, including quercetin and catechins, contribute to the vibrant colors of many fruits and vegetables. They include:
- Flavonols (e.g., quercetin in onions, apples, and kale),
- Flavones (e.g., luteolin in peppers and celery),
- Flavanones (e.g., hesperidin in citrus fruits),
- Flavan-3-ols (e.g., catechins in tea, cocoa, and apples),
- Anthocyanins (e.g., in berries and red wine),
- Isoflavones (e.g., genistein in soy and soy products), are known for their estrogen-like effects and potential benefits for heart health.
2. Phenolic Acids: This group includes hydroxybenzoic and hydroxycinnamic acids, which are present in foods like whole grains, coffee, and some fruits, phenolic acids, such as ferulic acid and caffeic acid, offer protective effects against oxidative stress. They are crucial components of a balanced diet.
3. Polyphenolic Amides: Though less well-known, polyphenolic amides, like capsaicin in chili peppers, exhibit anti-inflammatory and antioxidant properties. Their inclusion in our diet adds an extra layer of health benefits.
4. Stilbenes: These polyphenols are found in small quantities in the diet, with resveratrol from red wine and grapes being the most prominent. Stilbenes are researched for their potential in promoting heart health and longevity.
5. Lignans: Found in seeds (particularly flaxseeds), whole grains, and vegetables, lignans are known for their phytoestrogenic properties and may contribute to reduced risk of certain types of cancer.
6. Tannins: Tannins, including hydrolysable tannins (like ellagitannins in pomegranates and gallotannins in tea) and condensed tannins (proanthocyanidins in berries, chocolate, and wine), are known for their astringent properties and health benefits, such as reducing blood pressure and anti-inflammatory effects.
Sources of Polyphenols – From Garden to Glass
Polyphenols are abundant in various plant-based foods, creating a spectrum of dietary options to harness their benefits:
- Fruits and Vegetables: Berries, apples, citrus fruits, and colorful vegetables are rich sources of polyphenols.
- Beverages: Tea, especially green tea, coffee, and red wine provide a delightful dose of polyphenols.
- Nuts and Seeds: Almonds, walnuts, and flaxseeds contribute to polyphenol intake.
- Whole Grains: Incorporating whole grains like oats and barley adds phenolic acids to your diet.
Antioxidant Role – Shielding Cells from Oxidative Stress
Polyphenols act as powerful antioxidants, neutralizing free radicals that can cause cellular damage. By scavenging these free radicals, polyphenols contribute to the prevention of oxidative stress, a key factor in various chronic diseases.
Emerging Prebiotic Role – Nourishing the Gut Microbiome
Beyond their antioxidant prowess, polyphenols have garnered attention as emerging prebiotics. Prebiotics are essential non-digestible fibers that feed the beneficial bacteria residing in our gut. Polyphenols foster a hospitable environment for these microbes, promoting a thriving and balanced gut microbiome.
Basics of Prebiotics and Their Gut Health Benefits
In the vast and intricate world of nutritional science, prebiotics emerge as critical yet often overlooked components of a healthy diet. Their role in fostering a beneficial gut microbiome is paramount, offering a cascade of health benefits that extend well beyond the confines of the digestive system.
What Are Prebiotics?
Prebiotics are a specific type of non-digestible fiber that act as fuel for the beneficial bacteria in our gut. Unlike their counterparts, probiotics, which are live beneficial bacteria, prebiotics help stimulate the growth and activity of these microbes without being digested or absorbed themselves. Upon reaching the colon, prebiotics are fermented by the gut microbiota, leading to the production of short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate. These SCFAs are pivotal for gut health, playing roles in nourishing colon cells, maintaining the integrity of the gut barrier, and modulating the immune system. Before delving into the specific benefits of prebiotics for gut health, it’s crucial to understand the fundamentals of these non-digestible fibers and their role in cultivating a flourishing gut ecosystem.
Types of Prebiotics

The diversity of prebiotic fibers reflects the complexity of the gut microbiome they support. Here’s the list of prebiotic types:
- Inulin: Found in foods like chicory root, garlic, and leeks, inulin is a complex carbohydrate that resists digestion in the small intestine and reaches the colon intact, where it becomes a feast for beneficial bacteria.
- Fructooligosaccharides (FOS): Present in fruits and vegetables like bananas, onions, and asparagus, FOS is another prebiotic that promotes the growth of beneficial gut bacteria, improving mineral absorption and possibly reducing levels of harmful cholesterol.
- Galactooligosaccharides (GOS): Derived from lactose, GOS is known for its positive effects on gut health, particularly in enhancing the growth of Bifidobacteria.
- Resistant Starch: Found in cooked and cooled potatoes, green bananas, and grains, resistant starch escapes digestion in the small intestine and ferments in the colon, producing SCFAs that benefit colon health.
- Pectin: Commonly found in apples, oranges, and carrots, pectin is fermented by the gut microbiota, leading to the production of SCFAs and promoting gut health.
- Beta-glucans: Present in oats, barley, and certain mushrooms, beta-glucans help lower cholesterol levels and enhance the immune response.
Gut Health Benefits of Prebiotics
Prebiotics, the dietary fibers that selectively nourish beneficial bacteria in the gut, offer a myriad of health benefits. Here’s a closer look at how they contribute to gut health:
- Enhanced Digestive Function – Prebiotics promote the growth of beneficial bacteria, which play a crucial role in breaking down food and absorbing nutrients. By increasing the population of these microbes, prebiotics help improve digestion and prevent common digestive issues, such as bloating and constipation.
- Strengthened Gut Barrier – The fermentation of prebiotics by gut bacteria produces short-chain fatty acids, like butyrate, which are essential for maintaining the integrity of the gut lining. A strong gut barrier prevents harmful substances from leaking into the bloodstream, protecting against inflammation and associated diseases.
- Balanced Microbiome – Prebiotics support a balanced gut microbiome by fostering an environment where beneficial bacteria can thrive. This balance is critical for suppressing the growth of pathogenic bacteria, and reducing the risk of infections and gut-related disorders.
- Boosted Immune Function – A healthy gut microbiome, supported by prebiotics, plays a vital role in the body’s immune response. By enhancing the gut flora, prebiotics help regulate the immune system, making it more efficient in fighting off infections and reducing the incidence of autoimmune diseases.
- Improved Nutrient Absorption – The action of beneficial bacteria, nurtured by prebiotics, is essential for the proper absorption of nutrients, such as calcium and magnesium. This improved absorption supports bone health, energy production, and overall well-being.
- Reduced Inflammation – By promoting a healthy gut microbiome and strengthening the gut barrier, prebiotics can help lower systemic inflammation, which is linked to a host of chronic conditions, including heart disease and diabetes.
- Enhanced Mental Well-being – Emerging research suggests a strong link between gut health and mental health, often referred to as the gut-brain axis. Prebiotics, by supporting gut health, may have a positive impact on mental well-being, potentially alleviating symptoms of depression and anxiety.
By incorporating prebiotic-rich foods into your diet, such as garlic, onions, bananas, and whole grains, you can enjoy these comprehensive benefits for gut health and beyond.
Probiotics vs. Prebiotics – Distinguishing Roles
It’s crucial to differentiate between probiotics and prebiotics. While probiotics introduce live bacteria into the gut, prebiotics foster the growth of existing beneficial bacteria.

Both are integral to gut health, working synergistically for optimal digestive function.
How do Polyphenols Benefit the Gut Microbiome?
Polyphenols, naturally occurring compounds found in plants, are celebrated for their extensive health benefits, particularly for the gut microbiome. Their complex interaction with the gut ecosystem contributes to enhanced gut health through multiple biological pathways.
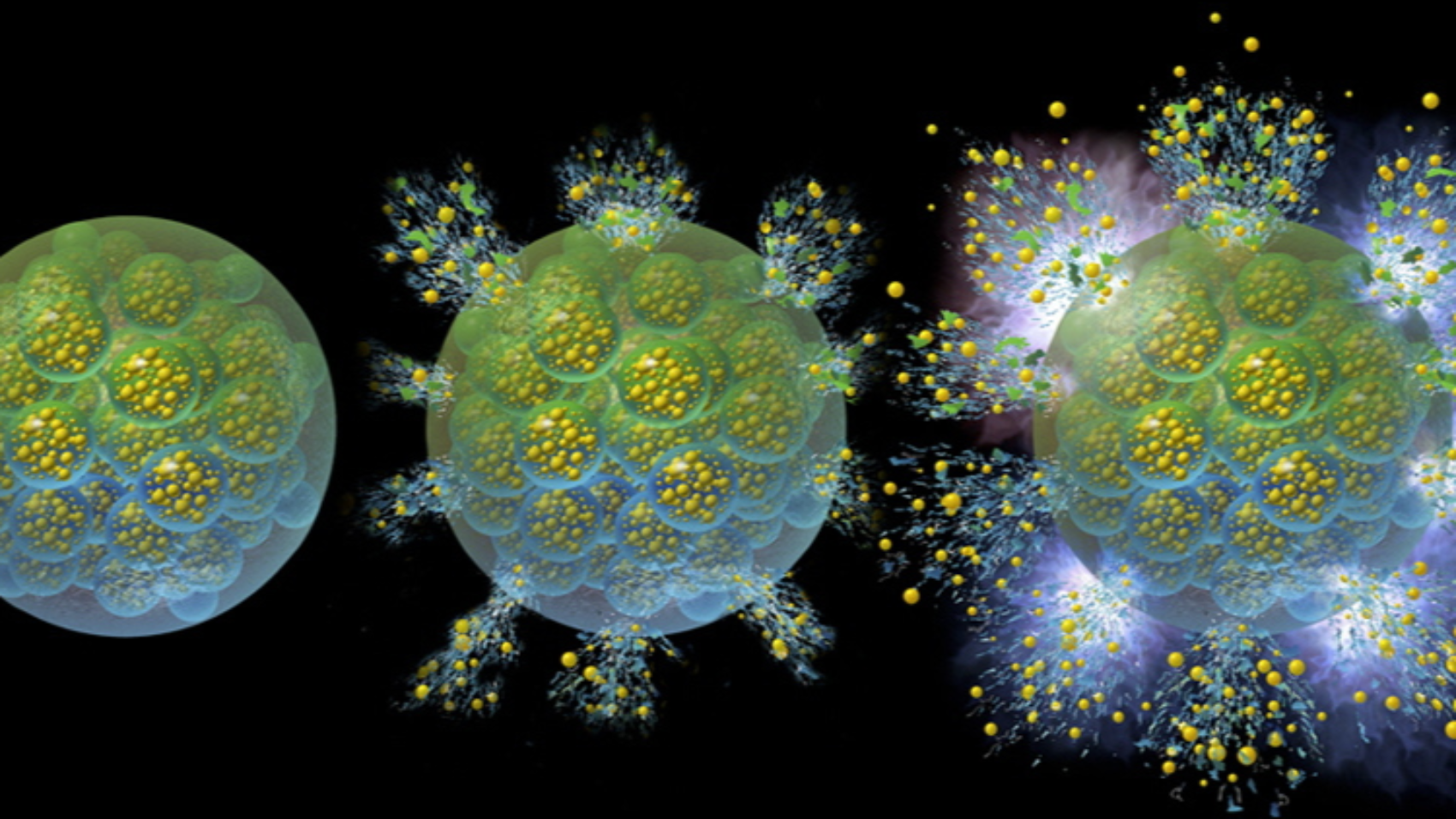
1. Antimicrobial Effects
One of the primary ways polyphenols benefit the gut microbiome is through their antimicrobial properties. Polyphenols can suppress pathogenic bacteria while promoting the growth of beneficial bacteria, such as Lactobacilli and Bifidobacteria. This selective antibacterial action helps maintain or restore balance within the gut ecosystem, crucial for digestive health and immune function.
- Selective Inhibition: Polyphenols interfere with the growth of harmful bacteria by disrupting their cell membranes or inhibiting their enzyme activity. This selective inhibition ensures that beneficial bacteria can thrive and dominate the gut environment.
- Biofilm Disruption: Some pathogenic bacteria form protective biofilms that enhance their resistance to antibiotics. Polyphenols can disrupt these biofilms, making the bacteria more vulnerable to natural immune responses and beneficial microbial competition.
2. Antioxidant Properties
Polyphenols are potent antioxidants, capable of scavenging free radicals and reducing oxidative stress in the gut. This antioxidant action is beneficial for gut health in several ways:
- Protecting Gut Lining: By neutralizing free radicals, polyphenols help protect the cells lining the gut from oxidative damage. This protection helps maintain the integrity of the gut barrier, preventing leaky gut syndrome and associated inflammatory responses.
- Modulating Inflammation: Polyphenols can modulate the immune system’s response, reducing chronic inflammation within the gut. This is particularly beneficial for conditions like inflammatory bowel disease (IBD), where inflammation plays a key role.
3. Enhancing SCFA Production
The fermentation of polyphenols by gut bacteria results in the production of short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate. SCFAs are crucial for gut health, serving several important functions:
- Energy Source for Colon Cells: SCFAs, particularly butyrate, are a primary energy source for colonocytes (the cells lining the colon), supporting their health and function.
- Strengthening Gut Barrier: SCFAs help reinforce the gut barrier, reducing permeability and the risk of pathogens entering the bloodstream.
- Regulating Immune Response: SCFAs modulate the immune system, promoting tolerance and preventing inappropriate inflammatory responses that can lead to autoimmune conditions.
Polyphenol-Rich Foods

Incorporating polyphenol-rich foods into your diet is a powerful way to boost your overall health, particularly benefiting the gut microbiome. Here’s a guide to some of the best sources of polyphenols to consider for your meals:
- Berries: Strawberries, blueberries, raspberries, and blackberries are loaded with anthocyanins, a type of polyphenol known for its antioxidant properties.
- Nuts and Seeds: Almonds, hazelnuts, pecans, and flaxseeds are excellent sources of polyphenols. They also offer healthy fats and fiber, enhancing their gut health benefits.
- Vegetables: Spinach, onions, and artichokes are not only nutrient-dense but also high in polyphenols. The diverse range of vegetables available allows for varied dietary intake.
- Fruits: Apples, cherries, plums, and grapes, particularly those with dark skins, are rich in various polyphenols, including flavonoids and resveratrol.
- Legumes: Black beans, red beans, and lentils are great plant-based protein sources and are packed with polyphenols.
- Whole Grains: Whole grains like oats, barley, and whole wheat contain lignans and other polyphenols, contributing to a healthy gut and reducing inflammation.
- Spices and Herbs: Cloves, peppermint, and star anise are among the spices and herbs with the highest polyphenol content. They can significantly boost the polyphenol content of any dish.
- Tea and Coffee: Green tea, black tea, and coffee are well known for their high polyphenol content, particularly flavonoids in tea and chlorogenic acids in coffee.
- Dark Chocolate and Cocoa: Rich in flavanols, dark chocolate, and cocoa products offer cardiovascular and brain health benefits in addition to their gut health-promoting properties.
- Olive Oil: Extra virgin olive oil is a staple in the Mediterranean diet, celebrated for its high content of polyphenols like oleuropein and hydroxytyrosol, which offer antioxidant and anti-inflammatory benefits.
- Red Wine: Moderation is key, but red wine is a notable source of resveratrol and other polyphenols, contributing to heart health and potentially the gut microbiome.
Tips for Incorporating Polyphenols into Your Diet
- Diversity is Key: Aim for a wide variety of polyphenol-rich foods to ensure a broad spectrum of benefits.
- Think Colorful: Generally, the more vibrant the color of the food, the higher its polyphenol content, so fill your plate with colorful fruits and vegetables.
- Opt for Whole Foods: Processed and refined foods lose much of their polyphenol content, so choose whole, unprocessed options whenever possible.
- Be Mindful of Preparation: Some polyphenols can be lost during cooking. Whenever possible, eat fruits and vegetables raw or lightly cooked to preserve their polyphenol content.
By integrating these polyphenol-rich foods into your daily diet, you can enjoy a delicious and natural way to support your gut health and overall well-being.
Conclusion
In conclusion, the prebiotic benefits of polyphenols represent a captivating frontier in the pursuit of optimal gut health. By understanding the diverse roles of polyphenols, incorporating polyphenol-rich foods into your diet, and staying informed on ongoing research, you can begin a journey towards a resilient and flourishing gut microbiome.
Prioritize your gut health today for a healthier tomorrow.
It’s also crucial to acknowledge that personalized health plans can make all the difference. Dr. Rasha El Naggar, through her clinic, Etara Wellness, has been a guiding force in helping individuals create effective health strategies. Understanding the significance of polyphenols in your well-being is just the beginning, and Dr. Rasha is here to assist you in formulating plans customized to your unique needs.
For personalized insights and to begin your journey towards better health, don’t hesitate to reach out to Dr. Rasha El Naggar at Etara Wellness.
Your path to a healthier and more vibrant life is just a consultation away.
CLAIM YOUR 15 MINUTES FREE PHONE CALL
—————————————————————————————————————————————–
Disclaimer: This content is for educational purposes only and not intended as medical advice. Consult a healthcare professional for any medical concerns.
—————————————————————————————————————————————–
Dr. Rasha El Naggar, MD, Ms.Biotech, ND – Founder of Etara Wellness
Dr. Rasha El Naggar is a distinguished Naturopathic Doctor, who melds rigorous scientific training with a holistic approach to wellness. Her academic journey commenced at Ain Shams University, Egypt, where she was awarded her MD, followed by an MS in Biotechnology from Johns Hopkins University. Dr. El Naggar further honed her expertise in naturopathic medicine at Bastyr University, San Diego, embodying a profound commitment to integrative health practices.
Based in Orange County, California, Dr. El Naggar is renowned for her personalized care in hormonal regulation, weight management, gut health, mental well-being, and regenerative medicine. Her health challenges catalyzed her passion for naturopathy, fostering a deep empathy and a holistic methodology in patient care.
As the visionary behind Etara Wellness, Dr. El Naggar integrates ancient healing traditions with contemporary scientific evidence. Her mission is to empower individuals to achieve balance, vitality, and optimal health. Dr. El Naggar’s professional narrative is characterized by resilience, innovation, and a relentless pursuit of wellness, making her a vanguard in naturopathic medicine.